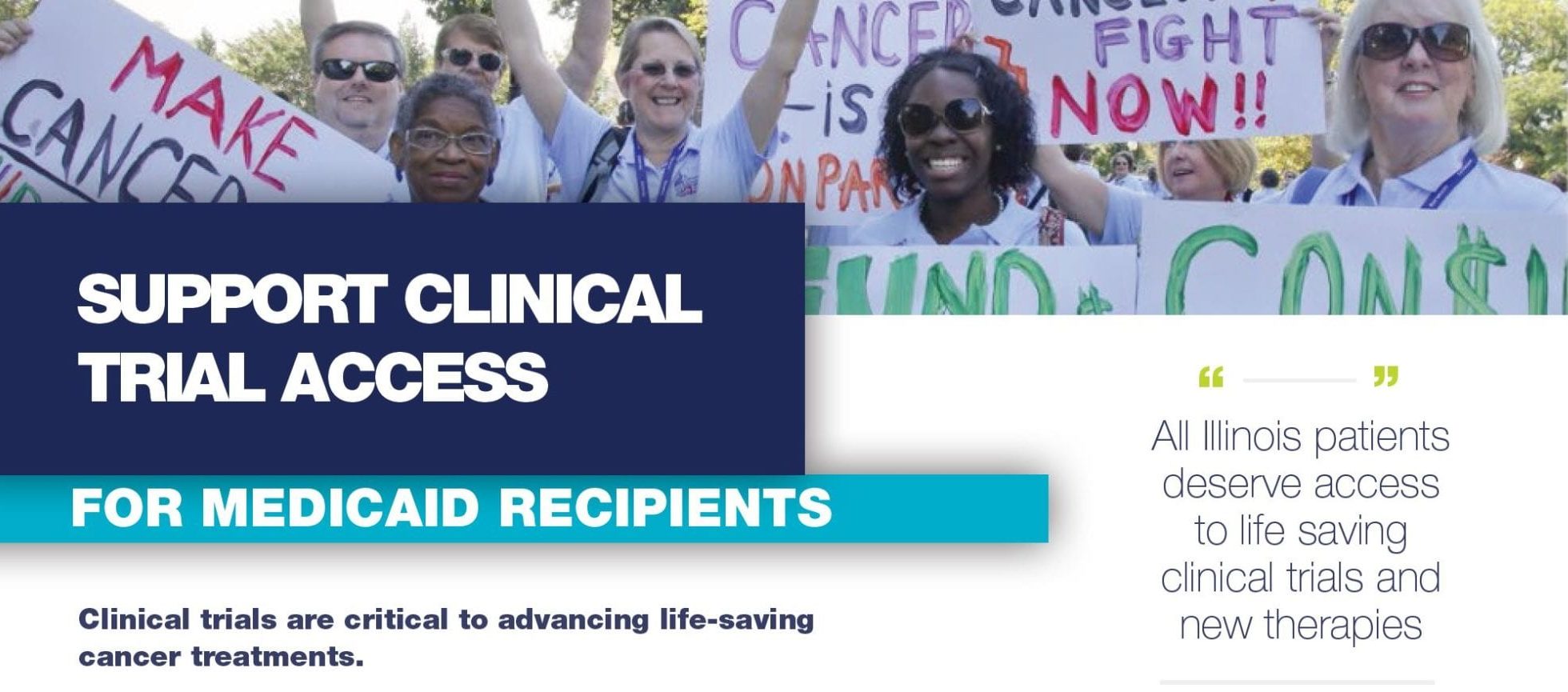
Support Clinical Trial Access for Medicaid Recipients
Patient participation in trials is crucial to this success. Currently Medicaid, the second largest insurance type in Illinois, is one of the few remaining insurance programs in the U.S. that is not required to cover routine care costs for
patients in cancer clinical trials. Although several states require Medicaid plans to offer this coverage, Illinois is not one of them.
WHAT DOES THIS MEAN?
Over 20% of Illinoisans do not have access to potentially lifesaving treatments offered through clinical trials due to lack of insurance coverage. Each year, more than 100 of our patients here at Illinois CancerCare are not considered for clinical trial enrollment due to Medicaid insurance restrictions. All patient should have access to every treatment option available, regardless of insurance coverage!
The American Cancer Society Cancer Action Network (ACS CAN) in partnership with Illinois CancerCare are taking ACTION in support of legislative change. A new senate bill (SB2499) was submitted on January 28, 2020 requesting that Medicaid cover all routine care costs regardless of clinical trial participation.
How Can You Help?
Register to join ACS CAN’s 2020 Virtual Illinois Day at the Capital – Tuesday, May 5th!
Cancer advocates from across the state will come together to use their voices to tell our lawmakers to make fighting cancer a top priority!
Learn More →
Become a member of ACS CAN
A nonprofit advocacy group dedicated to influencing change that positively impacts the future of cancer. this coverage, Illinois is not one of them.
Learn More →
Call your state Senator!
Ask your Senator to vote YES to improving access to clinical trials for Medicaid enrollees.
Find Your Senators Contact Information →